A narrative review of clinical studies on thread embedding acupuncture treatment for spasticity after stroke
Article information
Abstract
Objectives
This study aimed to review clinical studies on thread embedding acupuncture (TEA) for the treatment of patients with post-stroke spasticity (PSS)
Methods
Clinical studies related to TEA treatment for PSS were searched for in several electronic databases, including PubMed, Cochrane Library, MEDLINE, OASIS, and CNKI. After the selection/exclusion process, information on study design, disease, experimental/control group, intervention, outcome measurement, between-group differences, and adverse events was extracted.
Results
A total of 13 randomized controlled trials were included in this review. The usual frequency of TEA treatment was once every 1–2 weeks, and the treatment most commonly included 4 sessions. In the dorsal area, EX-B2 and the acupoints in governing vessel meridian were commonly used. Acupoints in the meridian of the large intestine were most frequently used in the treatment of upper limb spasticity. Except for HT1, PC6, and PC8, all TEA points for treating PSS of the upper limb were on the Yang meridians. For the lower limb spasticity, the most frequently used acupoints were ST36, GB34, GB30, BL60, and BL57 on Yang meridians, and LR3, SP6, SP9, and SP10 on Yin meridians. TEA treatment showed better effects than conventional treatment for PSS in terms of spasticity, motor dysfunction, and activities of daily livings. Nevertheless, the absence of the follow-up observation, lack of sham TEA treatment, and low quality of the included studies necessitated caution in interpreting the results.
Conclusions
The results of this review are expected to provide basic data on the modalities of TEA treatment for PSS and provide insights to facilitate well-designed studies in the future.
Introduction
Post-stroke spasticity (PSS), characterized by muscle stiffness, limited range of motion, and coordination disorder, is one of the most common complications of stroke. Although the pathogenesis of PSS has not yet been precisely elucidated, PSS is known to be a type of upper motor neuron syndrome caused by hyperexcitability of the stretch reflex1). PSS limits the performance of daily activities, such as eating, dressing, and washing, and increases the patient’s dependence of the patient on others, leading to substantially poorer quality of life2). Various treatments, including drugs, physical therapy, neurolysis, and botulinum neurotoxins, have been applied to relieve spasticity and suppress its progression, have been applied in clinical practice, but their safety and long-term effects have not been clarified3).
Thread embedding acupuncture (TEA) is a method of embedding suture threads made of catgut or polydioxanone thread into the acupuncture points. Since the continuous stimulation by the embedding thread is added to the effect of acupuncture, TEA treatment is preferentially applied to diseases with chronic and stubborn progress in clinical practice4–5). However, we were unable to find any clinical studies in Korea of TEA, nor any reports on the treatment status of TEA, in the treatment of PSS. In the clinical practice guideline of Korean Medicine for stroke developed in 2021, the use of acupuncture, electroacupuncture, pharmacopuncture, moxibustion, and herbal medicine is recommended for PSS6). However, recommendations in this guideline do not include TEA for the treatment of PSS.
Nevertheless, through an exploratory search for clinical studies conducted in China, it was found that TEA is widely applied as a single or combined therapy for PSS. In this study we performed a literature review of clinical studies on TEA published in foreign academic journals to investigate the utilization of TEA to treat PSS. The results of this study are expected to broaden the applications of TEA treatment for PSS and provide preliminary data to facilitate well-designed clinical studies in the future.
Materials and Methods
1. Search strategy and terms
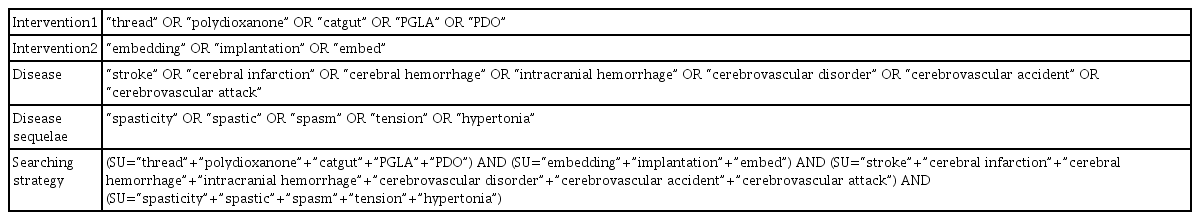
Clinical studies on TEA in the treatment of PSS were searched in foreign online databases, including PubMed, Cochrane Library, MEDLINE, Oriental Medicine Advanced Searching Integrated System (OASIS) and CNKI. Relevant search terms with Boolean operators (AND/OR) were combined and presented in Table 1.
2. Eligibility Criteria
Clinical studies that evaluating the effectiveness of TEA for PSS were included. Animal studies, review articles, protocols, and dissertations were excluded. The selection/exclusion process was conducted by comparing the results of searches performed independently by two investigators. If the eligibility did not match, the final inclusion was decided by the two researchers coming to an agreement. After excluding studies that did not meet the selection criteria through an initial review of the titles and abstracts, the full texts of the remaining studies were reviewed. Studies in which TEA was applied as part of a complex intervention along with other treatments were excluded if the effect of TEA could not be confirmed.
3. Data Extraction
The two investigators extracted and cross-checked data from the eligible studies. The extracted data included authors, year of publication, the number of participants, interventions, outcome measures, treatment periods and sessions, details on the TEA device used, acupuncture points, and adverse reactions. Additionally, we extracted the evaluation tool outcomes for spasticity, motor dysfunction, and daily life performance. If the information extracted from a selected study was inconsistent, a final decision was made through the two researchers reaching a consensus.
Results
1. The selection of eligible studies
A total of 27 potentially relevant clinical studies were retrieved through database searching. There were five studies found in PubMed, 21 in CNKI, and one in OASIS. Twenty-five studies were reviewed after excluding two duplicated studies. Nine studies were excluded by reviewing the title and abstract, of which six did not include human subjects and three were not related to TEA treatment. Through a full-text review, a total of 13 studies were finally obtained, excluding two studies that did not use evaluation tools for spasticity and one study found in OASIS, in which it was not confirmed that the subjects had PSS (Fig 1).
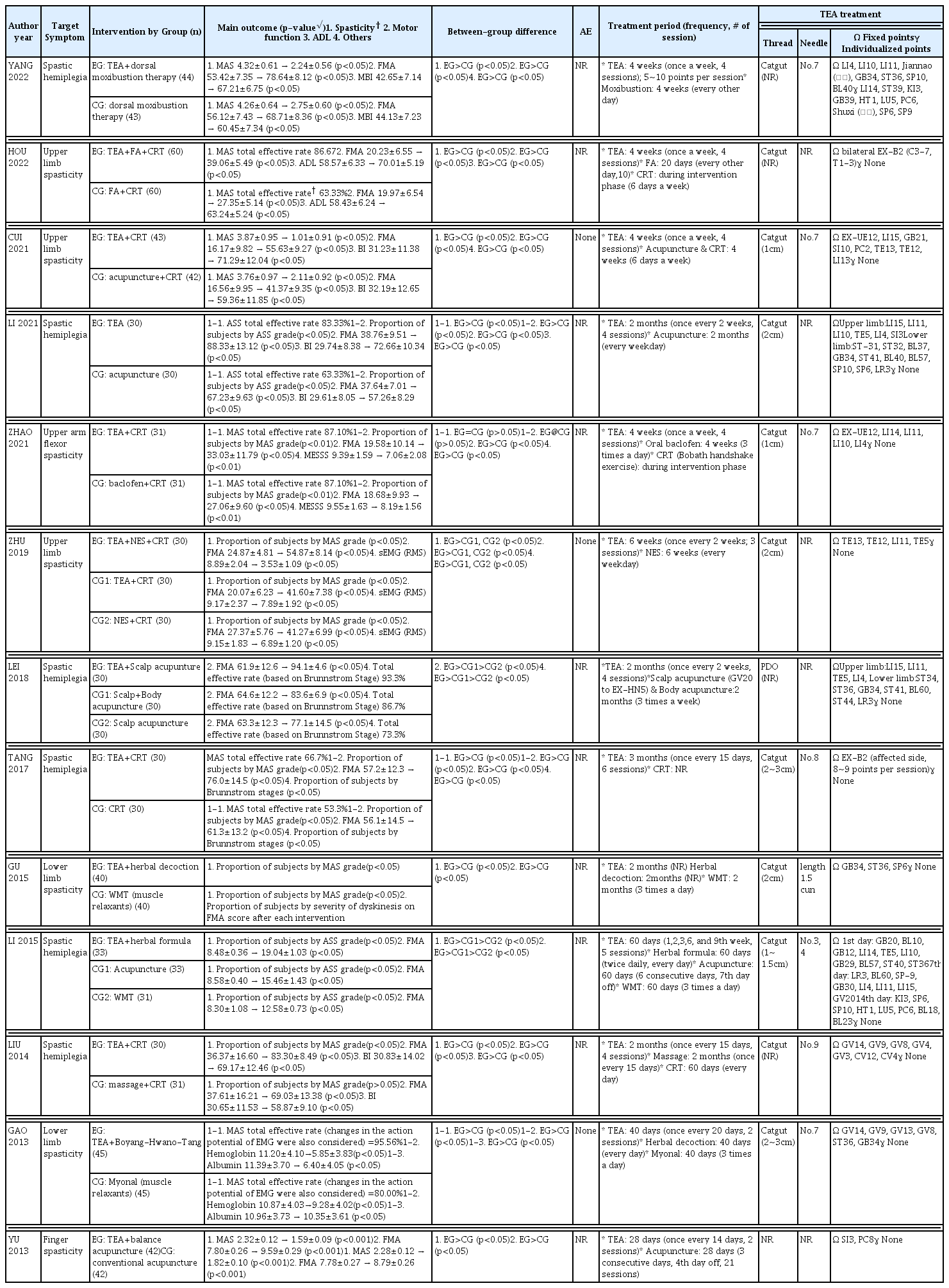
All 13 studies were randomized controlled trials conducted in China and were written in Chinese. Six studies focused on upper and lower limb spasticity, four on upper limb spasticity, two on lower limb spasticity, and one on finger spasticity. An overview of the selected clinical studies is shown in Table 2.
2. Intervention for the experimental/control group
There was one study (7.7%) in which TEA treatment was used as a single intervention in the experimental group, and 12 studies (92.3%) in which TEA treatment was used in combination with other Traditional Chinese Medicine treatments, such as acupuncture (n=3, 23.1%), herbal medication (n=3, 23.1%), and moxibustion (n=1, 7.7%), or with Western conventional medicine treatments (n=5, 38.5%), including rehabilitation treatment and nerve electrical stimulation. Regarding control group interventions, there were four studies (30.8%) that provided only Traditional Chinese Medicine treatment; five studies (38.5) used Western conventional treatment, such as medication and rehabilitation treatment, and the other four studies (30.8%) combined Traditional Chinese Medicine treatment and Western conventional treatment.
3. Outcome measures
As evaluation tools for spasticity, Modified Ashworth scale (MAS) was adopted in 10 studies and the Ashworth spasticity scale (ASS) in two studies. In the remaining study by LEI, 201813), the Fugl-Meyer motor assessment (FMA), which evaluates motor dysfunction due to spasticity and weakness, was used as the primary outcome measure without MAS or ASS. In the study by GAO, 201318), hemoglobin and albumin levels in the blood were also used as the secondary endpoint for spasticity. In all 12 studies evaluating motor dysfunction, the FMA was adopted. Activities of daily living (ADL) were measured in five studies using the Barthel Index (BI), Modified Barthel Index (MBI), and ADL index. Other assessments included Brunnstrom stage, Modified Edinburgh–Scandinavian Stroke Score (MESSS), and surface electromyography (sEMG).
4. Overview of the study results
All experimental groups in the selected studies showed statistically significant within-group differences between before and after the allocated treatment. All the control groups in the selected studies were the active control groups, and significant within-group differences between before and after the treatment were found in all studies, except for the study by LIU, 201417), which applied massage and conventional rehabilitation treatment. In all studies, except for that by ZHAO, 202111), which compared TEA + conventional rehabilitation treatment (CRT) with oral baclofen + CRT for upper limb spasticity, the experimental groups showed statistically significant better improvements in spasticity, motor dysfunction, and ADL compared to the control group.
For spasticity, changes in the proportion of subjects by MAS or ASS grade were presented in four studies. In three studies, MAS was presented as mean±standard deviation, and the mean differences in MAS before and after the treatment are shown in Table 2. The remaining five studies presented the total effective rate, which was calculated as {markedly effective (decreased by > 2 grade) + effective (decreased by 2 grade) + improved (decreased by 1 grade)} / n × 100. The total effective rates in the experimental groups of the five studies ranged from 66.7% to 95.6%. Three studies (23.1%) reported no adverse events, and the remaining 10 studies (76.9%) did not report any adverse events post-TEA treatment.
5. Details of TEA treatment
In 13 studies, TEA treatments were performed an average of 3.83 times for an average of 6.54 weeks. Regarding the number of TEA treatments, seven studies (58.3%) had four sessions, two studies (16.7%) had two sessions, and three studies had three, five, and six sessions each. In one study, no information on TEA treatment sessions was reported. Regarding the frequency of TEA treatment, four studies (30.8%) performed treatment once a week, five studies (38.5%) every 2 weeks, one study (7.7%) with once every 20 days, one study (7.7%) used five sessions over 9 weeks, and two studies (15.4%) provided no information relating to the frequency. TEA needles of No. 3 to No. 9 were used, and suture thread materials were catgut (n=11, 84.6%), polydioxanone (n=1, 7.7%), and unspecified (n=1, 7.7%). There were two studies with suture thread lengths of 2–3 cm, two studies with 2-cm length, two studies with 1-cm lengths, one study with 1~1.5 cm, and five studies without information regarding thread length.
In four studies (30.8%), TEA treatment was performed on dorsal area acupoints, including EX-B2, GV4, GV8, GV9, and GV14. In nine studies (69.2%), TEA treatment focused on the acupoints of the affected extremities. The most frequently used acupoints in the upper limb were LI4, LI10, LI11; TE5 in the forearm; and EX-UE12, Jiannao (肩臑), LI14, and LI15 in the upper arm and shoulder region. Except for HT1, PC6, and PC8, all acupoints used in the upper limbs were on the Yang meridians. The most frequently used acupoints in the lower limb were ST36, GB34, GB30, BL60, and BL57 on the Yang meridians, and LR3, SP6, SP9, and SP10 on the Yin meridians.
Discussion
Treatment for PSS is controversial, because some argue that spasticity is beneficial in maintaining posture and preserving bone density and muscle mass20). However, treatment for spasticity is still needed because the disturbances in ADL and personal hygiene and deterioration in mobility impair the quality of life of the patients and their caregivers. Spasticity is also considered a risk factor for post-stroke pain, as stretching of contracted muscles acts as a noxious stimulus through muscle fibers disruption21). In the treatment of patients with PSS, non-pharmacological approaches, including stretching of the spastic muscles, neuromuscular electrical stimulation, electroacupuncture, and moxibustion, are usually combined with pharmacological approaches. Therefore, we conducted this study to review modalities of TEA treatment as a single or combined therapies for PSS so that this information may be utilized when designing future clinical research studies.
In terms of TEA treatment details, the usual frequency of TEA treatment was once every 1 to 2 weeks, and the most common TEA treatment session frequency was four sessions. The suture thread material in the selected studies was most commonly catgut, which is generally used in China. The size of the TEA needles in the studies ranged from No. 3 (0.3 mm diameter) to No. 9 (0.9 mm diameter). Considering that 26–30 gauge of TEA needles are commonly used in Korea, it was confirmed that thicker needles are used in China than in Korea. The length of the suture thread varied from 1 to 3 cm, and in China, the TEA treatment method involves the practitioner cutting the suture and combining it with a needle tip. In 12 of the 13 selected studies, TEA treatment was applied as a combined treatment, reflecting the clinical reality that TEA treatment is mainly applied in combination with other Korean Medicine treatments or Western conventional medicine.
Regarding the TEA points used in the studies, EX-B2 and acupoints in governing vessel (GV) meridian were commonly used in the dorsal area. In EX-B2, the TEA points corresponding to the level of the segment that dominate the affected upper or lower extremities were selected. Among the acupoints in the GV meridian, GV8, which is located below the spinous process of the ninth thoracic vertebra, has been used to relieve stiffness and spasm of muscles and tendons. GV14 is one of the acupoints known as the “seven acupoints for stroke” and has been found to improve cerebral blood flow in several studies22–24). Acupoints in the meridian of the large intestine are most frequently used in the treatment of upper limb spasticity. Except for HT1 in the axillary region and PC6 and PC8 in the medial forearm region, all TEA points for treating upper limb spasticity in the included studies were on the Yang meridians. A study by Sim, 200325) also found that electroacupuncture on the acupoints of the Yang meridians were more effective than electroacupuncture on those of the Yin meridian in the treatment of elbow spasticity after stroke. In contrast, in the lower extremities, the TEA points in the Yang and Yin meridians were utilized to a similar degree. The most frequently used acupoints in the lower limb were ST36, GB34, GB30, BL60, and BL57 on the Yang meridians, and LR3, SP6, SP9, and SP10 on the Yin meridians. TEA treatment of both the flexor and extensor muscles may be effective in treating lower limb spasticity, but additional research is needed to establish scientific evidence for this.
In the assessments of PSS by MAS or ASS grades, the total effective rate was adopted most frequently. The total effective rate in the studies was defined as the sum of the number of subjects divided by the total number of subjects in each case. Classifications were as follows: markedly effective (decreased by > 2 grade), effective (decreased by 2 grade), and improved (decreased by 1 grade). The total effective rates of the experimental groups of the five studies were ranged from 66.7% to 95.6%. However, other studies present the results for PSS as the mean±standard deviation or the proportion of subjects by MAS/ASS grade, which causes difficulties in quantitatively synthesizing the results of these studies. In the included studies, TEA treatment in the experimental groups showed better improvements than those in the control groups in terms of spasticity, as well as motor dysfunction and ADL. This is thought to be because the improvement in PSS after TEA treatment has a positive effect on motor function and performance of activities of daily life.
However, two main limitations commonly found in the selected studies make it difficult to confirm the clinical effect of TEA in the treatment of PSS. First, none of the studies evaluated the persistence of the effect of TEA treatment through follow-up observations after the intervention phase. In the treatment of PSS, one of the factors thought to contributed to the superiority of TEA over conventional Korean Medicine treatment is the long-term and continuous stimulation by the embedded threads. However, no studies collected data on changes in the degree of spasticity during the follow-up period to evaluate the effect of this factor. Second, none of the studies used sham TEA as an intervention. By comparing real TEA to sham TEA in which there is no suture thread attached to the needle, the magnitude of the effect due to the embedded thread in PSS can be measured. However, no sham TEA device was used in any of the included studies. In addition, information on the randomization procedure, allocation concealment, and blinding of outcome assessment (detection bias) was not reported in the most studies.
In this review of selected clinical studies, TEA treatment showed statistically better effects than conventional PSS treatment. However, caution was required in the interpretation because of the absence of the follow-up observation, lack of sham TEA treatment, and the low quality of the studies. Despite these limitations, the results of this review are expected to provide basic data on TEA treatment modalities for PSS and insights to facilitate large scale clinical studies in the future.
Acknowledgement
This work was supported by a 2-Year Research Grant of Pusan National University
Notes
Conflicts of interest
The authors have no conflicts of interest to declare.